The wellbeing of healthcare professionals has never been more critical, nor more precarious. In a field defined by high stakes, long hours, and emotional intensity, burnout has become an all-too-common reality. While the term itself is often used casually, burnout in healthcare is a serious, multifaceted issue that affects not only the individuals experiencing it but also the quality of care delivered to patients and the overall performance of healthcare organizations. Preventing burnout requires more than individual resilience; it demands systemic awareness, cultural shifts, and a commitment to sustainable practices that prioritize the health of those who care for others.
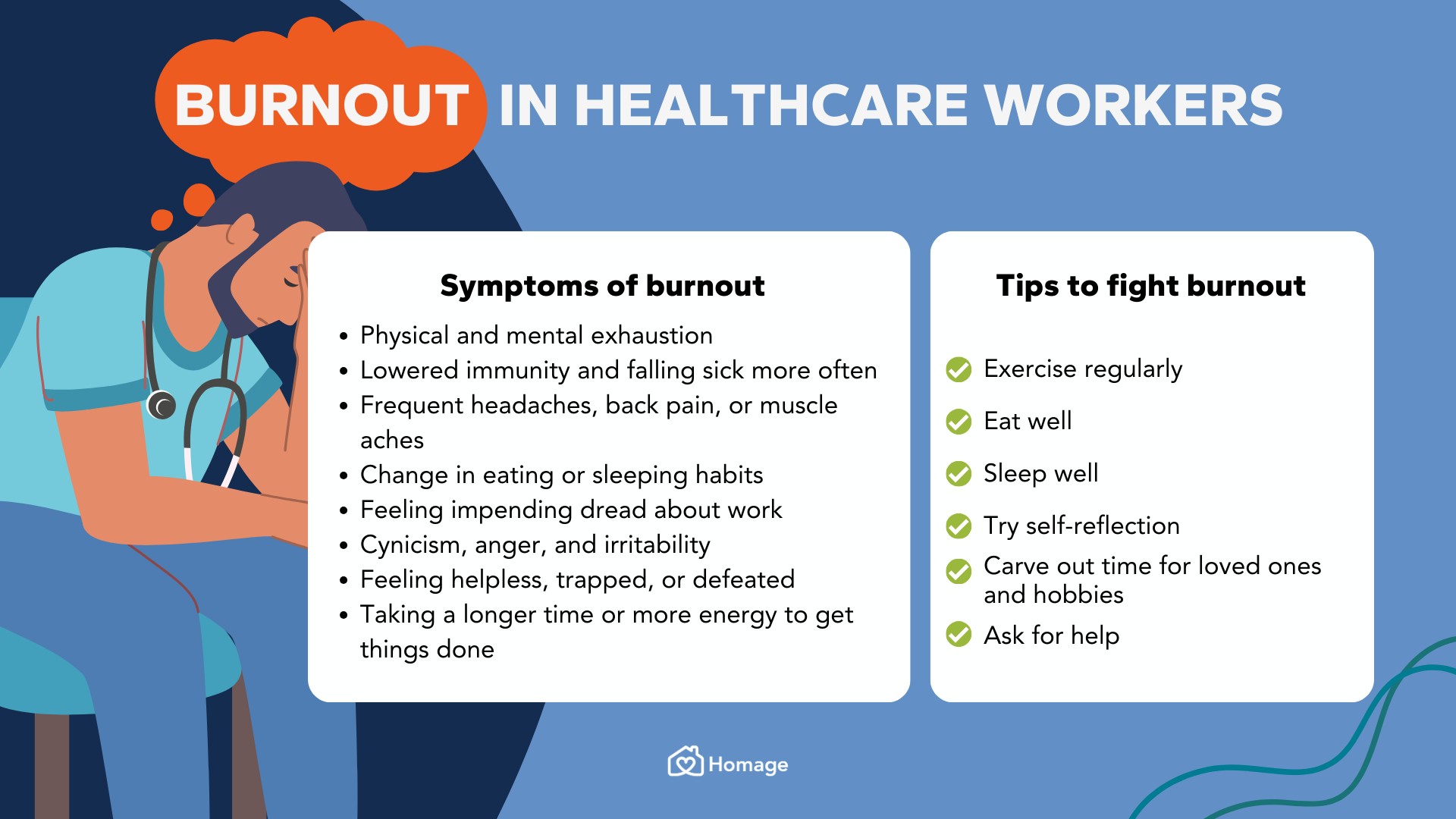
At its core, burnout is a response to chronic workplace stress that has not been successfully managed. It manifests in emotional exhaustion, depersonalization, and a diminished sense of personal accomplishment. For healthcare professionals, these symptoms are particularly dangerous. When a nurse becomes emotionally detached or a physician feels ineffective, the ripple effects can compromise patient safety, team dynamics, and organizational trust. The very qualities that draw individuals to healthcare—empathy, dedication, and a desire to make a difference—can become liabilities when not supported by a healthy work environment.
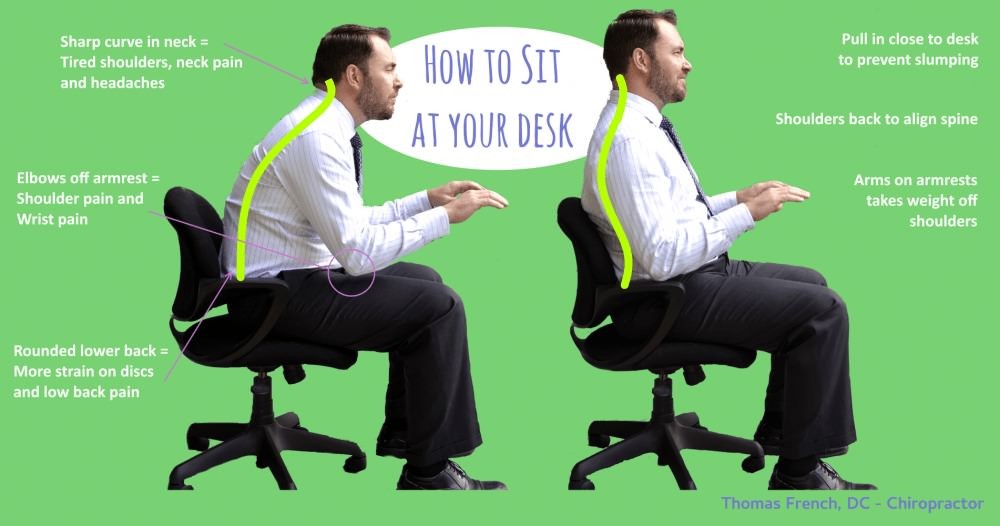
One of the most significant contributors to burnout is the relentless pace of modern healthcare. The pressure to see more patients, complete more documentation, and meet increasingly complex regulatory requirements leaves little room for recovery. Time that could be spent reflecting, learning, or simply breathing is often consumed by administrative tasks and back-to-back responsibilities. This constant demand erodes the mental and emotional reserves that professionals need to stay engaged and effective. Over time, what begins as fatigue can harden into cynicism, and what once felt like a calling can start to feel like a burden.
Addressing this issue requires a shift in how organizations view wellbeing. Too often, wellness initiatives are framed as optional add-ons—yoga classes, mindfulness apps, or occasional workshops. While these tools can be helpful, they are not sufficient on their own. True prevention of burnout must be embedded into the fabric of the workplace. This means rethinking workloads, ensuring adequate staffing, and creating systems that support rather than strain. It also means fostering a culture where asking for help is seen as a strength, not a weakness, and where mental health is treated with the same seriousness as physical health.
Leadership plays a pivotal role in setting the tone. When leaders model healthy boundaries, prioritize open communication, and actively listen to concerns, they create an environment where wellbeing is not just encouraged but expected. For example, a department head who regularly checks in with team members, not just about performance but about how they’re coping, sends a powerful message. That kind of presence builds trust and opens the door for honest conversations. It also helps identify early warning signs of burnout before they escalate into crises.
Peer support is another essential element. Healthcare can be isolating, especially in high-pressure roles where vulnerability is often masked by professionalism. Creating spaces for colleagues to connect, share experiences, and support one another can alleviate feelings of isolation and reinforce a sense of community. Whether through formal peer support programs or informal gatherings, these connections remind professionals that they are not alone in their struggles. They also provide opportunities to exchange coping strategies, celebrate small victories, and maintain perspective.
Technology, while often cited as a stressor, can also be part of the solution. Streamlining electronic health records, reducing redundant documentation, and leveraging automation for routine tasks can free up time and mental bandwidth. However, technology must be implemented thoughtfully, with input from frontline staff. Tools that are imposed without consideration for workflow can exacerbate stress rather than relieve it. The goal should be to enhance, not hinder, the human aspects of care.
Importantly, preventing burnout also involves supporting individual agency. Professionals need to feel that they have some control over their work—whether that’s through flexible scheduling, opportunities for professional development, or involvement in decision-making. Autonomy is a powerful antidote to helplessness, and when people feel empowered, they are more likely to stay engaged and committed. This sense of ownership can also drive innovation, as those closest to the work are often best positioned to identify improvements.
Ultimately, the wellbeing of healthcare professionals is not a luxury—it’s a necessity. It underpins the quality of care, the sustainability of the workforce, and the integrity of the healthcare system itself. Preventing burnout is not about eliminating stress entirely, which is neither realistic nor desirable. It’s about creating conditions where stress is balanced by support, where challenges are met with resources, and where the humanity of caregivers is honored as much as the needs of patients. In doing so, organizations not only protect their most valuable asset—their people—but also build a foundation for excellence that can endure even the toughest times.